Corneal Transplant
The cornea is the “window” into the eye. It is the front-most tissue of the eyeball, and is completely transparent under normal conditions. Its purpose is to help focus light, so you can have vision. If it is scarred, opacified, or swollen, then light is not properly focused into the eye. This results in blurry vision, glare, or both. If this cannot be treated with medication, repaired with other procedures, or healed further by your body, your ophthalmologist may recommend a corneal transplant.
A corneal transplant is when a diseased cornea is replaced with a clear cornea from a human donor. A donor is someone who chooses to donate their organs after their death (including their corneas). All donations are rigorously tested at a regional Eye Bank to ensure they are safe to use, and healthy enough to undergo transplantation.
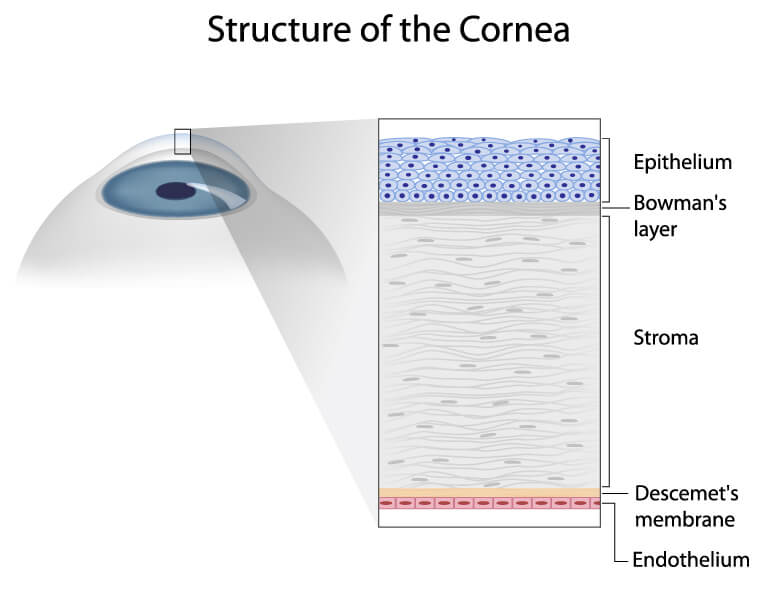
There are several different types of corneal transplants, depending on the layer of the cornea that is diseased. The cornea can be divided into five layers: epithelium (outermost, what your eyelid blinks over), Bowman’s layer, stroma, Descemet’s membrane, and endothelium (innermost). Sometimes, the entire cornea is replaced. Other times, only the innermost layers are replaced. In some cases, the front and middle layers only are replaced. Following any type of corneal transplant, you will most likely have to be on a low-dose steroid eye drop for the rest of your life to help prevent transplant rejection.
Types of Corneal Transplants
Penetrating keratoplasty (full thickness corneal transplant)
If the inner, middle, and outer layers are damaged (from infection, laceration, perforation, chemical burn, scar, or other conditions), then a penetrating keratoplasty (PKP) would need to be done to restore clarity to your line of sight. The entire thickness of the cornea is taken off, and the transplant is sewn into place. Your vision may take 12-18 months to “get back to normal” after a PKP. Sometimes, a specialty contact lens is needed to correct astigmatism following a PKP. The risk of rejection for a PKP is higher than other transplants, but still a low-risk overall.
Deep anterior lamellar keratoplasty
If the outer and middle layers of the cornea are damaged (from a partial-thickness scar, some keratoconus, or other various corneal dystrophies), then a DALK can be performed. This is very similar to a PKP, but your own Descemet’s membrane and endothelium (inner layers) are left behind. The advantage to this is quicker healing, and less chance of rejection as compared to PKP.
Endothelial keratoplasty
If the inner layer (the endothelium) is damaged (from Fuchs’ dystrophy, following cataract or glaucoma surgery, other corneal dystrophies, or other conditions), then the cornea can swell, causing blurry vision. It may be needed to replace just the inner layers of the cornea. There are two types of endothelial keratoplasty.
- DSEK (or DSAEK): Descemet’s stripping (automated) endothelial keratoplasty is where diseased Descemet’s membrane and endothelium are removed, and Descemet’s membrane, endothelium, plus a little stroma are floated-in on an air bubble to attach to the inside surface of the cornea. Because less of the cornea is disrupted, only a couple stitches are needed to close the wound, and chance of rejection is less, when compared to a PKP. For the first 24 hours after a DSEK, you would need to lay face-up at least 45 minutes of every hour to help with graft attachment. Rarely, the graft would need to be “repositioned” (another surgery) if it slips out of place. In general, visual recovery following a DSEK can take about 3-6 months (sometimes less, sometimes more).
- DMEK: Descemet’s membrane endothelial keratoplasty is similar to DSEK, however, Descemet’s membrane and endothelium only are transplanted. Since the transplanted tissue is much thinner, visual recovery is quicker than DSEK (typically about 1-2 months, sometimes a little more). However, the thinner tissue makes the surgery more technically challenging, and also requires 72 hours of face-up positioning. Furthermore, the chance of needing a “re-bubbling” (another procedure) to help the transplant fully attach is higher for DMEK than DSEK.
Your ophthalmologist will help counsel you on which endothelial transplant is best for your circumstances.